Signed in as:
filler@godaddy.com
Signed in as:
filler@godaddy.com
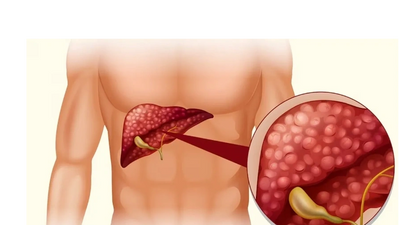
Cirrhosis is a serious condition where normal liver tissue is replaced by scar tissue (fibrosis). It tends to progress slowly and often does not cause symptoms in its early stages. However, as the function of the liver gradually becomes worse, serious problems can develop.
In the UK, the two commonest causes of cirrhosis are alcohol drinking above recommended limits and hepatitis C infection. Treatments may vary, depending on the cause. If cirrhosis becomes severe, a liver transplant may be the only option.
In this article:
What is cirrhosis of the liver?
Cirrhosis is a condition where normal liver tissue is replaced by scar tissue (fibrosis).
The 'scarring' tends to be a gradual process. The scar tissue affects the normal structure and regrowth of liver cells. Liver cells become damaged and die as scar tissue gradually develops. Therefore, the liver gradually loses its ability to function well.
The scar tissue can also affect the blood flow through the liver, which can cause back pressure in the blood vessels which bring blood to the liver. This back pressure is called portal hypertension.
What does the liver do?
Liver function
The liver is in the upper right part of the tummy (abdomen). It has many functions which include:
Cirrhosis symptoms
In the early stages of the condition, there are often no symptoms of cirrhosis. Livers can continue to function with a reduced number of working liver cells. However, as more and more liver cells die and more and more scar tissue (fibrosis) builds up, the liver:
Therefore, the symptoms that may develop include:
The scar tissue restricts the flow of blood through the liver and, as the cirrhosis becomes worse, this causes back pressure in the portal vein (known as portal hypertension). The portal vein is the vein that takes blood from the gut to the liver - this is rich in nutrients and also carries any toxins that the liver should be removing from the body.
Increased pressure in this vein can cause swellings (varices) to develop in the branches of the vein in the lining of the gullet (oesophagus) and stomach. These varices have a tendency to bleed easily into the gut. If a bleed occurs, this may cause vomiting of blood or passing altered blood with your stools (faeces) - this tends to make the stools black, tarry and offensive (melaena).
What causes cirrhosis?
There are many causes of 'scarring' of the liver (cirrhosis). In the UK the most common causes are alcohol and infection with the hepatitis C virus.
Alcoholic cirrhosis
Liver cells break down alcohol but too much alcohol can damage the liver cells. As a rule, the heavier the drinking, the more the risk of developing cirrhosis. However, alcoholic cirrhosis is not just a condition of people who have alcohol dependency. People who are drink socially but above recommended limits also develop cirrhosis.
About 1 in 10 people drinking above the recommended alcohol limits will eventually develop cirrhosis. It tends to occur after 10 or more years of excessive drinking. It is not clear why some people are more prone to their liver cells becoming damaged by alcohol and to developing cirrhosis. There may be an inherited (genetic) tendency. Women seem to be more prone than men to cirrhosis although it is still a disease more common in men.
Hepatitis C and cirrhosis
Persistent (chronic) infection with the hepatitis C virus causes long-term inflammation in the liver. This can eventually lead to liver 'scarring' and cirrhosis. Up to 1 in 5 people with chronic hepatitis C develop cirrhosis but this usually takes about 20 years or even longer from the initial infection.
Other causes of cirrhosis
Causes which are less common in the UK include:
How common is cirrhosis?
There are an estimated 30,000 people living with cirrhosis in the UK and at least 7,000 new cases being diagnosed each year. The numbers of people living with both alcoholic cirrhosis and non-alcohol-related cirrhosis seem to be rising.
How is cirrhosis diagnosed?
A doctor may suspect, from symptoms and a physical examination, that there is 'scarring' of the liver (cirrhosis). A doctor may especially think of cirrhosis as a cause of these symptoms if you have a history of heavy alcohol drinking or have had a previous episode of hepatitis.
Blood tests may show abnormal liver function. See the separate leaflet called Liver Function Tests for more details. An ELF blood test can give a good estimation of the degree of fibrosis in the liver and whether further tests for cirrhosis are needed. An ultrasound scan (or a computerised tomography (CT) scan or a magnetic resonance imaging (MRI) scan) may show a damaged liver. To confirm the diagnosis, a small sample (biopsy) of the liver may be taken to be looked at under the microscope. See the separate leaflet called Liver Biopsy for more details. The scarring of the liver and the damage to liver cells can be seen on a biopsy.
If the underlying cause of the cirrhosis is not clear, further tests may be done to clarify the cause. This might involve checking for antibodies to hepatitis viruses, checking for autoantibodies that may have attacked liver cells, looking in a blood sample for excess iron or copper, etc.
Cirrhosis treatment
'Scarring' of the liver (cirrhosis) tends to become progressively worse if the underlying cause persists and is not treated. In general, once the damage is done the scarring is not reversible. Therefore, the aim of treatment is, if possible, to prevent further liver scarring or to slow the progression of the scarring process. Treatments that may be advised include the following.
Stop drinking alcohol
Whatever the cause of cirrhosis, alcohol should be stopped completely. Drinking alcohol will increase the rate of progression of cirrhosis from whatever cause.
Be cautious when taking medicines
It is important that a doctor or pharmacist is aware of the diagnosis of cirrhosis before taking any prescribed or over-the-counter medicines. Some medicines that are processed in the liver may need their dose adjusted and some should not be used at all.
Treatment for underlying causes
Some of the underlying causes of cirrhosis can be treated. This may slow down, or halt, the progression of cirrhosis. For example:
Treatment to ease symptoms and prevent complications
Various treatments may be advised, depending on the severity of the cirrhosis and the symptoms that develop. For example:
Treatment of bleeding varices
A bleed from swellings (varices) - described above - is a medical emergency. Seek medical help immediately if you have cirrhosis and:
Various surgical techniques can be used to stop the bleeding and to help reduce the risk of further bleeds.
Liver transplant
In severe cases, where the scarring is extensive and the liver can barely function, then a liver transplant may be the only option.
The future
Up until recently, the scarring process of cirrhosis was thought to be irreversible. However, recent research has led to a greater understanding of the scarring process. Some research suggests that medicines may be able to be developed that can reverse the scarring process.
Stem cell or liver cell transplantation aimed at restoring liver function is also being investigated. This research continues.
Can cirrhosis be prevented?
Alcohol
The most common cause of 'scarring' of the liver (cirrhosis) in the UK is alcohol drinking above recommended limits. The most important way to prevent cirrhosis from developing is to drink within the recommended safe limits. That is:
Where do these recommendations come from?
In general, the more alcohol is drunk above these limits, the more harmful alcohol is likely to be.
A unit of alcohol is about equal to:
Note: using the above guide, it is easy to underestimate how much alcohol is in a drink. This is because many beers are now strong and wines are often served in 175 ml glasses. Many wines are also stronger than standard (some contain 12-14% alcohol by volume).
However, it is important not to drink alcohol at all if cirrhosis has already developed or with a diagnosis of chronic hepatitis or certain other liver problems.
Infectious diseases
Some causes of cirrhosis are due to infectious diseases which can often be prevented. For example, people who inject street drugs are at risk of hepatitis B and C if they use unclean needles or other injection equipment. These infections may also be passed on through unprotected sex. Hepatitis B can be prevented by immunisation which is offered to those at risk such as healthcare workers, drug users and people with multiple sexual partners.
We love our customers, so feel free to visit during normal business hours.
Rajiv Gandhi Circle, Sarvanand Nagar, Pipliya Rao, Indore, Madhya Pradesh
Open today | 06:00 pm – 08:00 pm |
We use cookies to analyze website traffic and optimize your website experience. By accepting our use of cookies, your data will be aggregated with all other user data.